Telehealth isn’t the newest healthcare advancement; however, COVID-19 is changing how it is used to treat patients. Telehealth is being utilized during the pandemic to combat the personal protective equipment (PPE) shortage, keep patients isolated and safe in their homes, which allows hospital beds to be open to the patients that really need them. Large companies like GM, Nike and Fanatics have joined the fight against COVID-19 and started producing health care equipment – from ventilators to PPE – to help combat the shortages.
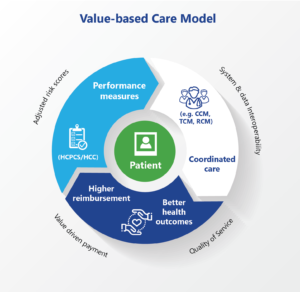
Value-based care model benefits patients, providers, payers and the community!
Even in the pandemic, quality measures and quality health care still matter and are at the forefront of patient care. Quality measures work to optimize health outcomes by improving quality and transforming the health care system. The measures are able work toward transforming health care because providers and their organization are monetarily credited for the ability to reduce the amount and probability for return visits. This is measured through “evidence-based and practice specific data in the categories of quality, improvement activities [that advance] care information and cost.” Centers for Medicare and Medicaid (CMS) updated the quality measures on January 29, 2020.
Are you utilizing quality measures to increase your reimbursement from payers? Failure to implement quality measures may result in reduced payments, lowering star ratings, removing insurer-allocated patients or canceling contracts.






