Quality healthcare is a high priority for the everyone in the industry, and CMS and commercial payers are transitioning to a value-based approach that pays (and rewards) providers and facilities for improving overall patient health and reducing the impacts of long term chronic disease.
This approach requires providers/facilities to quantify the quality of care given to a patient by providing specific data for each encounter using coding (CPT, DX, HCC and RxHCC codes) and HEDIS quality measures at time of claim submission.
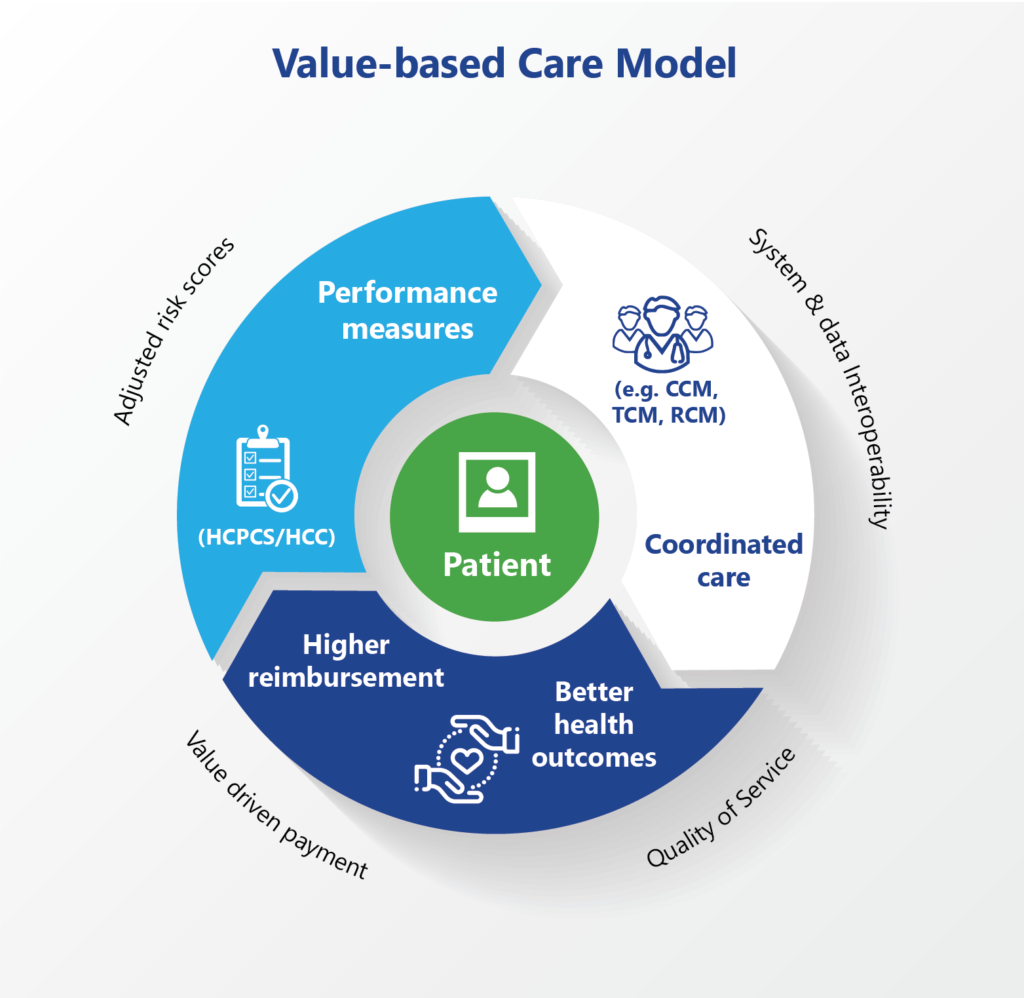
The data is then used by payers to get a full picture of the patient and treatment plan when enables them to determine a risk score for each patient and identify those with serious or chronic illness who are expected to incur greater medical cost. This is especially important for managed care plans, since this directly impacts the amount allocated per patient.
Payers reward facilities that provide detailed patient data and quality measures through higher reimbursement and opportunity to generate new revenue streams through pay-for-performance (P4P), star ratings and bonuses. Conversely, payers will penalize facilities who do not provide adequate quality measures by reducing payments, lowering star ratings or even potentially removing insurer-allocated patients or cancelling contracts.
Are you ready to take advantage of the revenue opportunities that quality measures can offer for minimal effort? Don’t wait to the last minute!!
We can analyze your data and provide customized training – from coding to systems and process.







1 Comment. Leave new
[…] Payments are now being tied to provider performance and quality of patient care instead of volume (value-based care model) which is changing the way community health centers generate revenue today. With the cost of care […]